Therapy for Complex Trauma in Duncan, BC and Online Across Canada
Trauma can have a profound impact on our lives, influencing our mood and emotions, sense of self, and relationships with others. I specialize in working with trauma, particularly developmental or childhood trauma. If you grew up in a home that was unpredictable or at times felt unsafe, it likely affects the way you navigate the world as an adult.
If you find yourself stuck in patterns of self-criticism, pessimism, difficulty in relationships, and/or unstable moods - trauma therapy can help.
How does trauma show up?
Trauma can impact people in wide-ranging ways, and those impacts often make sense when we understand trauma as something that overwhelms the nervous system and our capacity to cope. The effects can show up immediately, or emerge months or years later, sometimes in subtle ways.
Here are some of the most common areas trauma can affect:
Nervous system & body
Chronic fight/flight (anxiety, hypervigilance, panic)
Freeze or shutdown (numbness, dissociation, fatigue)
Sleep difficulties, chronic pain, headaches, GI issues
Heightened startle response or feeling constantly “on edge”
Emotions
Difficulty regulating emotions (big swings or feeling flat)
Persistent fear, shame, guilt, or anger
Feeling overwhelmed by seemingly small stressors
Emotional numbing or difficulty accessing feelings at all
Thoughts & beliefs
Negative core beliefs (“I’m unsafe,” “Something is wrong with me,” “I’m not enough”)
Self-blame or harsh inner criticism
Difficulty concentrating, remembering, or making decisions
Intrusive memories or rumination
Relationships & attachment
Difficulty trusting others or feeling safe with closeness
People-pleasing, fawning, or over-functioning in relationships
Pulling away, isolating, or avoiding intimacy
Strong reactions to perceived rejection or conflict
Sense of self & identity
Disconnection from needs, wants, or boundaries
Feeling fragmented or “not like myself”
Shame-based identity rather than a coherent self-story
Difficulty knowing who you are outside of survival roles
Daily functioning
Burnout, exhaustion, or reduced capacity
Avoidance of places, tasks, or situations
Difficulty with work, school, or routines
Cycles of overdoing it followed by collapse
An important note
Two people can live through the same traumatic experience and be impacted in very different ways. Even siblings growing up in the same home can respond differently based on their individual nervous system, temperament, role in the family, and the meaning they made of what happened. Each nervous system adapts in the way it needs to survive. Different responses don’t mean one person was hurt more or less, or one person is “weaker”; they simply reflect different ways of surviving.
It’s important to note that the symptoms described above were once adaptive responses, developed to help us survive. With safety, support, and trauma-informed care, nervous systems can heal, patterns can soften, and capacity can grow.
What does trauma therapy look like?
There are many different approaches to trauma therapy, and the most effective one depends on you and the kind of trauma you’ve experienced.
For single-incident trauma — such as an accident or assault — structured approaches like Eye Movement Desensitization and Reprocessing (EMDR) can be very effective. When trauma is more chronic or relational in nature, such as growing up in an unsafe or unstable home or experiencing intimate partner violence, deeper, relational approaches are often more helpful. My approach to trauma treatment integrates attachment-based therapy, Internal Family Systems, and somatic work.
Historically, many trauma treatments were based on exposure or re-experiencing. The idea was that repeatedly revisiting traumatic memories in a safe environment would reduce their emotional intensity over time. Approaches that include this component include Cognitive Processing Therapy (CPT), Narrative Exposure Therapy (NET), Trauma-Focused Cognitive Behavioural Therapy (TF-CBT), and EMDR.
As trauma therapy has evolved, many clinicians now recognize that revisiting traumatic memories is not always necessary — and for some people, it can be counterproductive or even re-traumatizing. Janina Fisher, for example, developed the Trauma-Informed Stabilization Treatment (TIST) model, which emphasizes stabilization and nervous system safety rather than memory exposure.
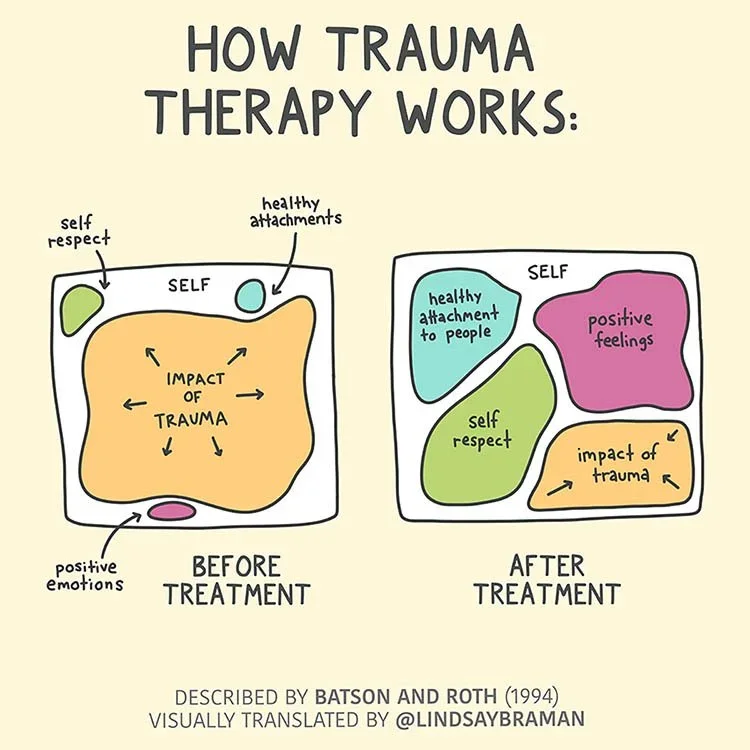
I love this image by Lindsay Braman. It reflects the idea at the heart of the NeuroAffective Relational Model (NARM): the persisting problem isn’t the trauma itself, but the survival strategies we developed to cope with it — strategies that often persist long after the danger has passed.
We can’t change what happened to you. But we can work with, understand, and gently shift the survival strategies that are no longer needed in your adult life.
In my approach to trauma therapy, the first step is developing a steady, attuned relationship where even the most vulnerable parts of you feel safe to emerge. Together, we explore the strategies different parts of you learned to rely on. These might include people-pleasing, perfectionism, pushing others away, clinging tightly to others, or many others that once served an important purpose.
Rather than trying to get rid of these strategies, we approach them with curiosity and respect — asking why these parts believe these patterns are still necessary. Often, beneath these protective strategies are younger parts holding immense grief, anger, or sorrow. With care and support, these parts can begin to release what they’ve been carrying and reconnect with their natural, childlike qualities — playfulness, joy, creativity, and curiosity.
“I am not what happened to me. I am what I choose to become.”
— Carl JungGet In Touch
If you're interested in working together, please fill out this form, or you can click the button below to book a free 20-minute consultation.